 Written by: Cory Tyszka
Written by: Cory Tyszka
HOSPITALS
Many health care professionals are on the front lines of the COVID-19 public health crisis around the world, and although Arizona is not immune to the disease’s wide-ranging effects, State-initiated measures and voluntary hospital “load-balancing” have prevented Arizona hospitals from being overwhelmed by COVID-19 patients.
Governor Ducey first declared a Public Health State of Emergency on March 11, 2020. On March 19, 2020, Governor Ducey expanded the State of Emergency efforts by barring all elective, non-essential surgeries in order to help hospitals preserve personal protective equipment (PPE) and hospital capacity. Hospitals around the state also worked cooperatively to establish a plan for patient distribution (load-balancing) so that no one hospital would become overwhelmed, despite the financial repercussions of sending patients to competitor hospitals [1]. Although Arizona is still seeing 250-350 new COVID-19 cases per day, these mitigation efforts appear to have helped to keep hospitals from becoming overwhelmed with patients.
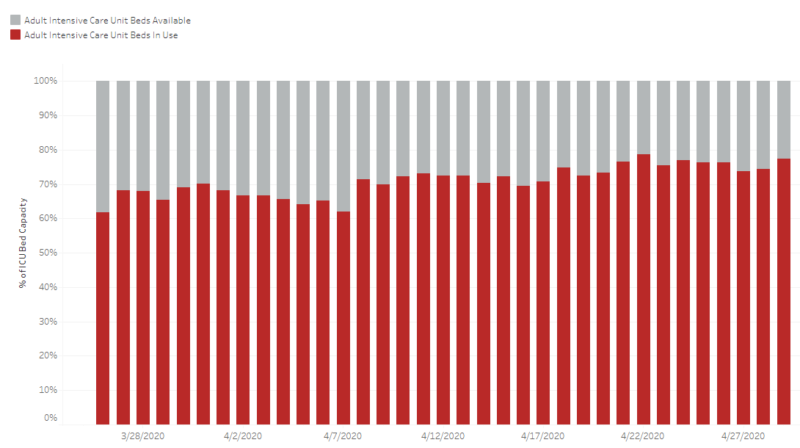
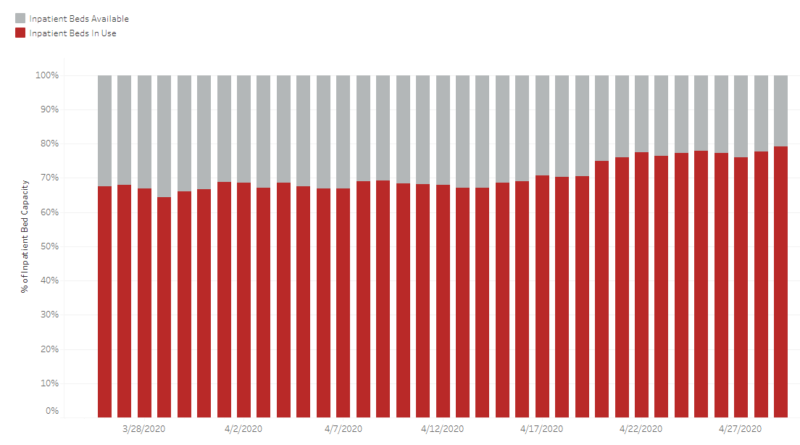
For the past month, Arizona hospitals have maintained availability of more than 20% of their ICU beds and approximately 20-30% of their inpatient beds.
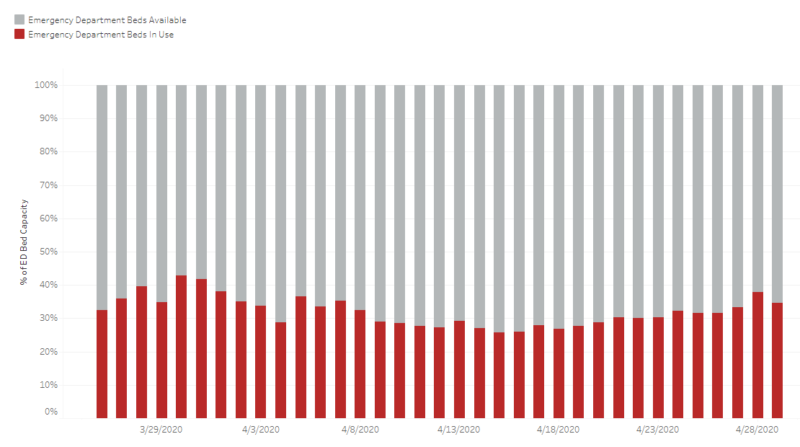
Emergency department bed availability has been maintained at well more than 50%.
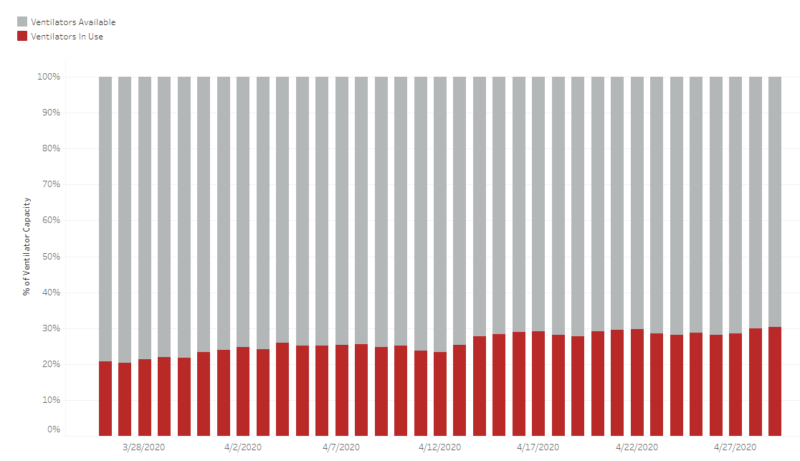
At least 70% of ventilators remain available for use if needed.
Because Arizona has avoided an overwhelming patient load, Governor Ducey relaxed the ban on elective surgeries by Executive Order on April 22, 2020. This Executive Order permits hospitals and other health care facilities to obtain an exemption to perform elective surgeries if the following conditions apply:
- Continuing supply of available PPE for minimum of 14 days;
- Minimum 20% hospital/facility bed availability;
- Enhanced hospital/facility cleaning procedures;
- Robust testing of all at-risk health care workers and each elective patient;
- Symptom screening of all staff, patients, and visitors prior to entering the hospital/facility;
- Pre-discharge testing of patients transferring to post-acute care facilities; and
- Prioritization of elective, non-essential surgeries consistent with Centers for Medicaid and Medicare Services guidelines.
The absence of elective surgeries, the reduction in trauma cases due to stay-at-home guidelines and recreational closures [2], and Governor Ducey’s Good Samaritan Executive Order providing for qualified immunity [3] for COVID-19 related health care services will inevitably result is less litigation arising out of hospital-provided medical care during this time frame.
TELEMEDICINE
With a reduction in hospital-based care, there has been an increase in telemedicine. This is therefore an area in which we might start to see an increase in litigation.
On March 25, 2020, Governor Ducey issued an Executive Order encouraging the use of telemedicine to the extent possible to prevent transmission of COVID-19 at health care facilities and protect at-risk populations and our health care professionals. Under the Executive Order, telehealth services may be provided through telephone or videoconference, and a patient’s home is an approved location to receive telemedicine. The patient’s insurance is required to cover the telehealth services to the same extent as if the visit had occurred in person. Prescriptions – even those that ordinarily require an in-person examination prior to issuance – may be written based on a telemedicine examination.
However, telemedicine is not without its challenges. Limitations include the inability to physically examine the patient, the inability to observe the subtle patient cues that the health care professional would otherwise appreciate in an office visit, and the potential inability to have the patient’s undivided attention in a busy home environment. Health care professionals might want to consider reviewing telemedicine best practice guidelines to help mitigate these limitations. These will help the practitioner identify the type of patient appropriate for telehealth services, implement appropriate technology for the scope of their practice, and establish practice procedures to ensure a meaningful doctor-patient exchange [4]. It remains to be seen whether telemedicine will continue to have broad usage after we get beyond the current public health crisis now that its commonplace practice has increased its acceptance.
______________
[1] Source: https://www.azfamily.com/news/continuing_coverage/coronavirus_coverage/az-hospitals-in-financial-crisis-with-fewer-patients-despite-more-covid-19-cases/article_91616ec8-7de4-11ea-8651-b7db86ca3a2d.html
[1] Gross negligence or reckless or willful misconduct, including rendering services under the influence of alcohol or an intoxicating drug is not protected under the Executive Order.
[1] See, e.g., American Telemedicine Association’s Quick-Start Guide to Telehealth during a Health Crisis.
Cory Tyszka focuses her practice in the areas of medical malpractice and health care liability defense, products liability, and wrongful death and personal injury defense. She represents all manner of medical service providers—including hospitals, physicians and nurses—as well as pharmaceutical and supplement manufacturers. She earned a B.A. in Biology from Wheaton College (MA), and continued her medical academic career in the Cancer Biology Interdisciplinary Program at the University of Arizona. Cory also has experience as a research technician at the Memorial Sloan-Kettering Cancer Center.